Implementation of GINA guidelines in Ho Chi Minh City: a model for Viet Nam.
Setting: The Global Initiative for Asthma (GINA) guidelines have not been implemented effectively in primary care settings in Viet Nam.
Objectives: To estimate the proportion of patients with controlled asthma and the direct health care costs of managing asthma according to GINA guidelines at four out-patient clinics in Ho Chi Minh City (HCMC), Viet Nam.
Methods: One hundred and six patients with asthma were treated and followed up according to GINA guidelines for 12 months. Clinical and pulmonary function responses and direct health care costs were evaluated every 3 months during the study.
Results: The proportion of patients with controlled asthma rose from 1.0% at the start of the study to 36.8% by the end of the study (P < 0.0001). The proportion of patients who had at least one hospitalisation per year decreased significantly, from 32.1% to 5.7% (P < 0.0001). The annual per patient median direct health care cost was US$169. Using asthma controllers continuously gave better asthma control than using them intermittently (OR 12.9, 95%CI 4.7–35.7).
Conclusions: The implementation of GINA guidelines at out-patient clinics in HCMC, Viet Nam, improved asthma control with modest direct health care costs.
Asthma is a chronic respiratory disease that has been increasing in prevalence over the past 30 years, particularly in low and middle-income countries. Some 235 million people worldwide suffer from this non-communicable disease.1 The Global Initiative for Asthma (GINA) guidelines were created to help physicians diagnose and manage asthma based on patients’ symptoms and spirometric results.2 The guidelines also underline the importance of treating stable but persistent asthma by using controller medications with minimal side effects to control symptoms and prevent exacerbations.
GINA guidelines need to be implemented in Viet Nam, especially at primary health care centres, because most patients with asthma first seek health care at these centres. However, primary care physicians at these centres have historically managed asthma using outdated treatment approaches, often only prescribing reliever medications (short-acting bronchodilators) when patients have asthma attacks and under-prescribing controller medications. Consequently, the proportion of patients with controlled asthma in Viet Nam is about 2.9%,3 which falls markedly short of the goal of asthma control for all patients specified in the GINA recommendations.4,5 Implementation of the GINA guidelines is therefore likely to be helpful.
The outcomes of implementation of the GINA guidelines in Viet Nam have not been published previously. The present study was conducted to estimate the proportion of patients with controlled asthma and the direct health care cost of managing asthma according to the GINA guidelines for 12 months at four out- patient clinics in Ho Chi Minh City (HCMC).
STUDY POPULATION, DESIGN AND METHODS
Setting
This prospective observational follow-up study was conducted from February 2007 to August 2008 at four out-patient clinics of the Health Care Centre of Hoc Mon District (Hoc Mon), the Health Care Centre of Phu Nhuan District (Phu Nhuan), the Regional General Hospital of Thu Duc District (Thu Duc) and the University Medical Centre (UMC) in HCMC. All are public health care centres. The first three are district- level health care centres, while the UMC respiratory out-patient clinic functions as a primary care clinic and a model of asthma management in the community in Viet Nam. The staff of this clinic was responsible for training health care workers and monitoring GINA implementation at the three other clinics during the study.
Patients had to pay for asthma controller medications because they were not covered by health insurance at the time of the study.
Patients
All asthma patients aged >15 years of age attending the above four clinics from February to June 2007 were identified. Only patients who had had asthma symptoms for more than one year and had not previously been managed according to GINA guidelines were invited to participate in the study.
The definitive diagnosis of asthma was based on recurrent attacks of cough, wheezing, chest tightness and dyspnoea, with spirometric results showing a change in forced expiratory volume in one second (FEV1) of ⩾200 ml (or ⩾12%) after inhalation of 400 μg salbutamol. Patients with persistent asthma who had not used controller medications while in a stable state were classified as having not previously been managed according to GINA guidelines.
The study was approved by the ethics committee of the HCMC Department of Science and Technology. Written informed consent was obtained from all subjects.
Implementation and data collection
Two doctors and two nurses at each of the participating centres attended a 2-week training course at the UMC in HCMC. In this hands-on course, participants were trained to perform spirometry, interpret spirometric results, diagnose and classify asthma, counsel patients with asthma and prescribe medications following GINA guidelines.
All patients were treated according to GINA guidelines and were followed up for 12 months. The last visit of the last patient for this study was in August 2008.
At the first visit, all patients underwent a complete medical history interview and physical examination. Comorbidities, asthma drugs ever used and number of hospitalisations in the preceding year were based on patient recall. Plain chest X-rays were taken to exclude infectious lung diseases, and spirometry was performed before and 15 min after inhalation of 400 μg salbutamol using the KoKo® spirometer (nSpire Health, Inc., Longmont, CO, USA). The spirometric manoeuvres met the American Thoracic Society/ European Respiratory Society quality standard criteria.6 Spirometric parameters were calculated as percentage of predicted values, based on the reference equation of the Intermountain Thoracic Society 1984.7 Levels of asthma control were determined based on GINA criteria.2
Controller medications consisted of an inhaled corticosteroid (ICS; fluticasone propionate or budesonide) for ICS-naïve patients with partly controlled asthma, or a combination of an ICS and a long-acting inhaled beta2-agonist (LABA; fluticasone/salmeterol or budesonide/formoterol) for those patients with partly controlled or uncontrolled asthma. The reliever medication was inhaled salbutamol. In addition to pharmaceutical treatment, patients were asked to avoid trigger factors and to undergo an annual flu vaccination.
Patients were provided with the mobile phone numbers of the responsible doctors to use if they had questions about their asthma management. They were also asked to fill in their diary sheets every day, and present them to the doctors at each follow-up visit. Patients were asked to return for follow-up every 3 months after the first visit. If a patient delayed in making an appointment for more than 2 weeks, health care workers telephoned to remind them. At each follow-up visit, patients were evaluated for clinical control, medication adherence and side-effects, and frequency of hospitalisation. Patients also completed an Asthma Control Test (ACT) questionnaire at each visit.8
To ensure that all patients were examined at the month 12, we repeatedly called those patients who had missed that appointment and arranged a new appointment that was convenient for them.
Direct health care costs were calculated based on patients’ records in their diary sheets, including costs for consultation and spirometry, asthma medications and emergency department visits or hospitalisation due to asthma attacks. The cost was converted into US dollars at a rate of 16 500 Vietnamese dong (VND) for US$1 (2007 exchange rate).
Poor adherence was defined as patients who temporarily stopped using prescribed controllers without consultation with the responsible doctor for 4–12 weeks at any time during the study.
Some results of this study have been published elsewhere in abstract form.9
Statistical analysis
Data collected at each participating centre were entered by a doctor at that centre using Excel software (Microsoft Excel, Palisade Corp, Newfield, NY, USA) and were checked onsite regularly by another doctor from the UMC. The data were sent to the UMC for analysis.
The proportion of patients with at least one hospitalisation per year between the year of study and the preceding year, and the proportion of patients with controlled asthma or with ACT > 19 between each follow-up visit and the first visit, were compared using McNemar’s test. Spirometric parameters between each follow- up visit and the first visit were compared using paired Wilcoxon’s signed rank test.
Statistical analyses were performed using JMP 9.0.2 software (SAS Institute Inc., Cary, NC, USA). P < 0.05 was considered statistically significant.
RESULTS
Of 132 patients with asthma recruited on their first visit to four participating out-patient clinics in HCMC, 26 (19.7%) withdrew from the study within 3 months after the first visit because they could not afford asthma controllers. Statistical analyses were performed for 106 patients: 23 (21.7%) from the UMC, 28 (26.4%) from Phu Nhuan, 29 (27.4%) from Thu Duc and 26 (24.5%) from Hoc Mon.
The median duration of asthma was 5 years (range 1–51). Patient characteristics at the first visit are shown in Table 1. According to GINA criteria, only one (1.0%) patient had controlled asthma at the start of the study. Before participating in the study, 66 (62.3%) only used bronchodilators such as salbutamol when they had an asthma attack. Worryingly, 17 (16.0%) used an inexpensive, locally available oral combined generic medication (Asmacort®, F. T. Pharma, Ho Chi Minh City, Viet Nam) consisting of dexamethasone acetate, theophylline and phenobarbital, with a consequent risk of associated iatrogenic complications. This preparation was used before or during asthma attacks.
For the 12-month duration of the study, no oral asthma preparations were used. At the first visit, patients were started on inhaled controllers as follows: 92 (86.8%) on fluticasone/salmeterol, 9 (8.5%) on budesonide/formoterol and 5 (4.7%) on fluticasone propionate.
TABLE 1 Baseline characteristics of patients with asthma at four clinics in Ho Chi Minh City, Viet Nam, N = 106
|
Characteristic |
n (%) |
|
Age, years, mean ± SD |
46.0 ± 15.6 |
|
Female |
58 (54.7) |
|
Education level |
|
|
High school degree or higher |
55 (51.9) |
|
Smoking status |
|
|
Current smoker |
12 (11.3) |
|
Ex-smoker |
22 (20.8) |
|
Non-smoker |
72 (67.9) |
|
Comorbidities |
|
|
Allergic rhinitis |
26 (24.5) |
|
Chronic sinusitis |
17 (16.0) |
|
Gastroesophageal reflux |
7 (6.6) |
|
Past asthma drugs |
|
|
Inhaled corticosteroids |
23 (21.7) |
|
Systemic corticosteroids |
17 (16.0) |
|
Only bronchodilators |
66 (62.3) |
|
Levels of GINA-defined asthma control at first visit |
|
|
Under control |
1 (1.0) |
|
Partly under control |
8 (7.5) |
|
Not under control |
97 (91.5) |
|
⩾1 hospitalisation in the previous year |
34 (32.1) |
SD = standard deviation; GINA = Global Initiative for Asthma.
TABLE 2 Controlled asthma as defined by GINA during the study
|
Visit |
Examined n |
Asthma under control |
Missed appointment n (%) |
||
|
n |
% |
95%CI |
|||
|
First |
106 |
1 |
1.0 |
0.2–5.2 |
0 |
|
Month 3 |
101 |
29 |
28.7* |
20.8–38.2 |
5 (4.7) |
|
Month 6 |
82 |
22 |
26.9* |
18.4–37.3 |
24 (22.6) |
|
Month 9 |
69 |
22 |
31.9* |
22.1–43.6 |
37 (34.9) |
|
Month 12 |
106 |
39 |
36.8* |
28.2–46.3 |
0 |
* P < 0.0001 compared to the first visit.
GINA = Global Initiative for Asthma.
The number of patients who attended follow-up visits was 101 (95.3%) at month 3, 82 (77.4%) at month 6, 69 (65.1%) at month 9 and 106 (100%) at month 12. The proportion of patients with GINA-defined controlled asthma during the study increased significantly and consistently from month 3 until month 12 compared to the first visit (P < 0.0001 for all comparisons, Table 2). Levels of asthma control during the 12 months of the study are shown in the Figure.
Among those patients who completed the ACT questionnaire, the proportion of patients with ACT >19 at month 3 (36/60, 60.0%, 95% confidence interval [CI] 47.4–71.4), month 6 (33/54, 61.1%, 95%CI 47.8–73.0), month 9 (34/44, 77.3%, 95%CI 63.0– 87.2), and month 12 (75/98, 76.5%, 95%CI 67.2–83.8), was significantly higher than at the first visit (14/102, 13.7%, 95%CI 8.4– 21.7; P < 0.0001 for all comparisons).
The proportion of patients hospitalised at least once during the 12 months of the study (6/106, 5.7%, 95%CI 2.6–11.8) was significantly lower than in the preceding year (34/106, 32.1%, 95%CI 24.0–41.5; P < 0.0001).
The percentages of forced vital capacity (FVC%), FEV1, and peak expiratory flow (PEF%) during the study are shown in Table 3. FVC%, FEV1%, and PEF% had increased significantly at month 12 compared to the first visit (P = 0.0035, P < 0.0001, and P < 0.0001, respectively).
The median direct health care cost for managing asthma according to the GINA guidelines was US$169 per patient per year (1st–3rd quartile US$114–$237).
The rate of adherence was low, at 50% (53/106). Reasons for stopping the controllers were resolution of symptoms (23/53, 43.4%), inability to pay for the controllers (15/53, 28.3%), lack of health insurance reimbursement (10/53, 18.9%), fear of side effects of ICS (4/53, 7.5%) and other (lack of time, lack of transport and lack of awareness about the need for regular use, 10/53, 18.9%). After the 1-year study there was a significantly higher proportion of patients with controlled asthma among those who used controllers continuously (33/53, 62.3%) than among those who used them intermittently (6/53, 11.3%; OR 12.9, 95%CI 4.7–35.7).
TABLE 3 Spirometric parameters measured during the study
|
Visit |
Participants n |
Missed appointment n (%) |
FEV1 % predicted (95%CI) |
PEF % predicted (95%CI) |
FVC % predicted (95%CI) |
|
First |
106 |
0 |
71.8 (67.5–76.1) |
61.9 (56.9–66.8) |
84.4 (80.5–88.4) |
|
Month 3 |
99 |
7 (6.6) |
79.6 (75.1–84.1) |
74.5 (68.9–80.1) |
89.1 (84.8–93.5) |
|
Month 6 |
60 |
46 (43.4) |
76.6 (70.9–82.3) |
71.2 (64.3–78.1) |
86.0 (80.0–91.9) |
|
Month 9 |
48 |
58 (54.7) |
77.4 (70.5–84.2) |
68.2 (61.5–74.8) |
86.7 (80.2–93.3) |
|
Month 1 |
106 |
0 |
79.7 (75.2–84.2)* |
72.3 (67.3–77.3)* |
88.1 (84.0–92.3)† |
* P < 0.0001, †P < 0.01, compared to first visit.
FEV1 = forced expiratory volume in one second; CI = confidence interval; PEF = peak expiratory flow; FVC = forced vital capacity.
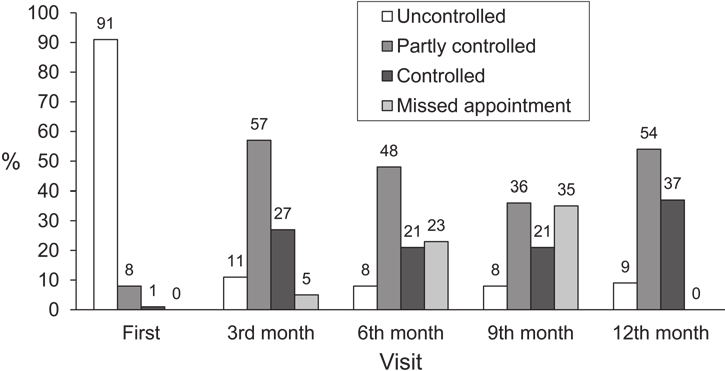
FIGURE Levels of asthma control after the introduction of Global Initiative for Asthma guidelines at four clinics in Ho Chi Minh City, Viet Nam.
DISCUSSION
After the implementation of GINA guidelines at four out-patient clinics in HCMC, mostly district-level centres, patients used more appropriate therapy and stopped using oral combined medications, minimising the incidence of treatment-related side effects. This study also shows that after one year of appropriate management, the proportion of patients with controlled asthma had improved significantly (P < 0.0001, Table 2), the proportion of patients hospitalised at least once per year had decreased significantly (P < 0.0001) and the direct health care cost was relatively low. This progress in the management of asthma patients thus partly met the GINA goals.
The proportion of patients with controlled asthma among patients using ICS in Europe in 1999–2002 was only 15%,10 while the proportion of patients with ACT > 19 was 45% among patients using ICS/LABA in a previous study from the United States.11 The higher proportion of controlled asthma or ACT > 19 in our study could be due to the fact that most patients used ICS/ LABA or ICS with GINA-recommended dosages, while patients from the two other studies might have used controllers with lower dosages than recommended. However, the proportion of patients with controlled asthma in our study was lower than in the Gaining Optimal Asthma controL (GOAL) study (41% after one year of intervention).12 In the GOAL study, for those patients who could not reach the target of totally controlled asthma with GINA- recommended doses of ICS/LABA, the authors prescribed long- term oral corticosteroids to increase their chances of reaching the target
The reduction in the hospitalisation rate might be attributable to the use of ICS or ICS/LABA as controllers during the stable state.13 The improvement in FEV1% and PEF% at the end of the study (Table 3) again supports the benefits of managing asthma according to GINA guidelines. This is consistent with reports from the GOAL study12 and the study by Boskabady et al.14
The adherence rate in this cohort study was poor (50%), but consistent with reports from other authors (30–70%).15,16 There are two possible reasons for the low adherence rate: first, many patients with asthma believe that they have asthma only when they have symptoms, and tend to stop using controllers when the symptoms disappear.17,18 In our study, 43.4% of poorly adherent patients stopped taking their controller medications when their symptoms resolved. This was also the most common reason for non-adherence in the AIRIAP study (36.2%).19 Second, the price of the controllers is still relatively high for many Vietnamese patients, at US$15/month (US$180/year) for a patient with uncontrolled asthma. The GDP in Viet Nam was US$843.20 in 2007.20 This reason was also common in the ARIAP study (30.8%),19 and is mentioned in the Global Asthma Report 2011.1
The median direct health care cost in our study was lower than that reported in the United States (mean direct health care cost, US$3180) or in Europe (mean medical resource utilisation €549.8 for a controlled patient, and €1451.3 for a non-controlled patient).21–23 The lower direct cost in HCMC was due to the inexpensive health care services, cheaper medications and lower hospitalisation rate when the patients used controllers.3,13,24 The increased rate of controlled asthma in our study also contributed to the decrease in direct health care costs. This is in agreement with the findings in the AIRIAP study, which showed that the direct cost significantly decreased when the levels of asthma control based on ACT improved.5 From our study and the AIRIAP study, we might expect that the total cost for managing asthma according to GINA guidelines would be lower than the cost for treating asthma using non-standardised approaches. This needs to be clarified in further studies.
The participants in this study were representative of most patients with asthma who sought health care in a primary care setting in HCMC, Viet Nam. They had not been previously managed according to GINA guidelines for the following reasons: lack of trained physicians for GINA implementation; unavailability of spirometers at these centres; unawareness about the cost-effectiveness of asthma management among health care workers and the public; and lack of affordable controllers. The results of this study should be validated by future studies when this model of GINA implementation can be applied to other provinces in Viet Nam.
This study had some limitations. First, as there was no control group in the study, we could not control for confounders such as physicians’ clinical skills, patients’ educational level or income, frequency of visits, etc. Second, the outcomes of the study might be overestimated due to the Hawthorne effect, i.e., patients act differently when observed. Third, as some patients missed their regular visits or did not undergo spirometry at certain visits, this may partly affect the results of the study. However, with the within- subject analysis of outcomes over follow-up, the results are still valid.
In conclusion, GINA implementation at four out-patient clinics in HCMC, Viet Nam, led to good asthma control after hands- on training for health care workers, and this improvement was sustained for one year.
N. V. Tho,1,2 H. T. H. Loan,3 N. T. P. Thao,4 N. T. T. Dung,5 L. T. T. Lan2,6
1 Department of Tuberculo- sis and Lung Diseases, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Viet Nam
2 Respiratory Care Centre, University Medical Centre at Ho Chi Minh City, Ho Chi Minh City, Viet Nam
3 Health Care Centre of Phu Nhuan District, Ho Chi Minh City, Viet Nam
4 Health Care Centre of Hoc Mon District, Ho Chi Minh City, Viet Nam
5 Regional General Hospital of Thu Duc District, Ho Chi Minh City, Viet Nam
6 Department of Physiology, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Viet Nam
CORRESPONDENCE
Dr Nguyen Van Tho Respiratory Care Centre University Medical Centre at Ho Chi Minh City 215 Hong Bang Street District 5 Ho Chi Minh City, Viet Nam
Tel: (+84) 8 3859 4470 .E-mail: thonguyen0225@ gmail.com
ACKNOWLEDGEMENTS
The authors thank the staff at the Respiratory Care Centre, University Medical Centre, Ho Chi Minh City, at the Out-patient Clinics of the Health Care Centres of Phu Nhuan and Hoc Mon districts and the General Regional Hospital of Thu Duc district, for their contribution to this study. The authors also thank M Thomas, Primary Care Research, University of Southampton, UK, for providing English help and useful suggestions on the paper. This study was funded by the Ho Chi Minh City Depart- ment of Science and Technology. Conflict of interest: none declared.
KEY WORDS asthma; cost-effectiveness; management; out-patient
References
-
International Union Against Tuberculosis and Lung Disease. The global asthma report 2011. Paris, France: The Union, 2011.
-
Global Initiative for Asthma. Global strategy for asthma management and prevention. Updated 2007. GINA, 2007. http://www.ginasthma.org/guidelines- archived-2007-update-clean-copy.html Accessed October 15, 2008.
-
Lai C K, Ko F W, Bhome A, et al. Relationship between asthma control status, the asthma control test and urgent health-care utilization in Asia. Respirology 2011; 16: 688–697.
-
Lai C K, De Guia T S, Kim Y Y, et al. Asthma control in the Asia-Pacific region: the Asthma Insights and Reality in Asia-Pacific Study. J Allergy Clin Immunol 2003; 111: 263–268.
-
Lai C K W, Kuo S-H, Guia T D, Lloyd A, Williams A E, Spencer M D. Asthma control and its direct health care costs: findings using a derived Asthma Control TestTM score in eight Asia-Pacific areas. European Respir Rev 2006; 15: 24–29.
-
Miller M R, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338.
-
Kanner R E, Morris A H, Crapo R O, Gardner R M, ed. Clinical pulmonary function testing. A manual of uniform laboratory procedures for the intermountain area. 2nd ed. Salt Lake City, UT, USA: Intermountain Thoracic Society, 1984.
-
Nathan R A, Sorkness C A, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004; 113: 59–65.
-
Tho N V, Mai H S, Thao N T P, Dung N T T, Lan L T T. Applying Global Initiative For Asthma (GINA) and Global Initiative For Chronic Obstructive Lung Disease (GOLD) at district-level health care centers in Ho Chi Minh City. Respirology 2010; 15 (S2): 55–109 [Poster Discussion 01-02].
-
Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol 2007; 120: 1360–1367.
-
Peters S P, Jones C A, Haselkorn T, Mink D R, Valacer D J, Weiss S T. Real- world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based survey. J Allergy Clin Immunol 2007; 119: 1454–1461.
-
Bateman E D, Boushey H A, Bousquet J, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control study. Am J Respir Crit Care Med 2004; 170: 836–844.
-
Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000; 343: 332–336.
-
Boskabady M H, Rezaeitalab F, Rahimi N, Dehnavi D. Improvement in symptoms and pulmonary function of asthmatic patients due to their treatment according to the Global Strategy for Asthma Management (GINA). BMC Pulm Med 2008; 8: 26.
-
Clatworthy J, Price D, Ryan D, Haughney J, Horne R. The value of self-report assessment of adherence, rhinitis and smoking in relation to asthma control. Prim Care Respir J 2009; 18: 300–305.
-
Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130 (Suppl): 65S–72S.
-
Halm E A, Mora P, Leventhal H. No symptoms, no asthma: the acute episodic disease belief is associated with poor self-management among innercity adults with persistent asthma. Chest 2006; 129: 573–580.
-
Haughney J, Price D, Kaplan A, et al. Achieving asthma control in practice: understanding the reasons for poor control. Respir Med 2008; 102: 1681–1693.
-
Zainudin B M, Lai C K, Soriano J B, Jia-Horng W, De Guia T S. Asthma control in adults in Asia-Pacific. Respirology 2005; 10: 579–586.
-
The World Bank. GDP per capita (current US$). Washington, DC, USA: The World Bank. http://data.worldbank.org/indicator/NY.GDP.PCAP.CD/countries/ VN-4E-XN?display=graph Accessed June 2012.
-
Cisternas M G, Blanc P D, Yen I H, et al. A comprehensive study of the direct and indirect costs of adult asthma. J Allergy Clin Immunol 2003; 111: 1212– 1218.
-
Haahtela T, Tuomisto L E, Pietinalho A, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006; 61: 663–670.
-
Van Ganse E, Laforest L, Pietri G, et al. Persistent asthma: disease control, resource utilisation and direct costs. Eur Respir J 2002; 20: 260–267.
-
Adams R J, Smith B J, Ruffin R E. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax 2000; 55: 566–573.
Contexte: Les Directives de l’Initiative Mondiale pour l’Asthme (GINA) n’ont pas été mises en œuvre de manière efficiente dans les contextes de soins primaires au Viet Nam.
Objectifs: Estimer la proportion de patients dont l’asthme est bien contrôlé ainsi que les coûts directs des soins de santé liés à la prise en charge de l’asthme selon les directives GINA dans quatre polycliniques externes de Ho Chi Minh City (HCMC), Viet Nam.
Méthodes: On a traité et suivi pendant 12 mois selon les directives GINA 106 patients asthmatiques. Les réponses cliniques et fonctionnelles pulmonaires ainsi que les coûts directs des soins de santé ont été évalués tous les 3 mois au cours de l’étude.
Résultats: La proportion de patients dont l’asthme a été contrôlé n’était que de 1% au début de l’étude et a atteint 36,8% à la fin de l’étude (P < 0,0001). La proportion de patients ayant subi au moins une hospitalisation par an a diminué de manière significative, de 32,1% à 5,7% (P < 0,0001). Le coût direct annuel médian des soins de santé par patient a été de 169 US$. Le recours continu aux contrôleurs de l’asthme a obtenu un meilleur contrôle de l’asthme que le recours intermittent (OR 12,9 ; IC95% 4,7–35,7).
Conclusions: La mise en œuvre des directives GINA dans les polycliniques externes de HCMC, Viet Nam, améliore le contrôle de l’asthme et comporte de modestes coûts directs de soins de santé.
Marco de referencia: Las directrices de la Iniciativa Global para el Asma (GINA) no se han puesto en práctica eficazmente en los centros de atención primaria en Viet Nam.
Objetivos: Calcular la proporción de pacientes con asma compensada y el costo directo que representa prestar una atención sanitaria en conformidad con las directrices de la GINA, en cuatro centros de consulta externa en la Ciudad de Ho Chi Minh, en Viet Nam.
Métodos: Ciento seis pacientes con asma recibieron tratamiento y acudieron al seguimiento de conformidad con las recomendaciones de la GINA durante 12 meses. Durante el estudio se evaluaron cada 3 meses la respuesta clínica, la evolución de las pruebas de función respiratoria y los costos directos de la atención sanitaria.
Resultados: La proporción de pacientes con asma equilibrada fue solo 1,0% al comienzo del estudio y aumentó a 36,8% al final del mismo (P < 0,0001). La proporción de pacientes hospitalizados como mínimo una vez por año disminuyó de manera significativa de 32,1% a 5,7% (P < 0,0001). La mediana del costo directo anual de la atención sanitaria por paciente fue 169 dólares. La administración continua de los medicamentos contra el asma dio mejores resultados que su uso intermitente (cociente de posibilidades 12,9; IC95% de 4,7 a 35,7).
Conclusión: La aplicación de las directrices de la GINA en los centros de consulta externa en la Ciudad de Ho Chi Minh, en Viet Nam, me joró el tratamiento del asma y generó un costo sanitario directo moderado.